A Note on the Reduction in Surgical Site Infections, Cost Savings, and Reduced Environmental Impact of Single-Use, Sterile, Pre-Packaged Surgical Instruments by Dr. Joseph Haymore, DNP
Single-Use, Sterile, Pre-Packaged (SSP) surgical implants and instruments have the potential to significantly reduce Surgical Site Infections (SSIs) and improve patient throughput, providing both superior patient outcomes and substantial cost-savings. Furthermore—and contrary to common assumptions—literature addressing the use of SSP instruments demonstrates that they have a lower overall lifecycle environmental impact than reusable instruments.

Single-Use, Sterile, Pre-Packaged (SSP) surgical implants and instruments have the potential to significantly reduce surgical site infections and improve patient throughput, providing both superior patient outcomes and substantial cost-savings. Furthermore—and contrary to common assumptions—literature addressing the use of SSP instruments demonstrates that they have a lower overall lifecycle environmental impact than reusable instruments.
Single-Use Sterile Instruments Reduce Surgical Site Infections and Associated Costs
Surgical Site Infections (SSIs) pose a significant—and far too common—danger to patients. Approximately 6.6% of spinal fusion procedures result in a surgical site infection—4.9% of which are deep-incisional infections.[i][ii] Similarly, nearly 3% of total knee arthroplasty procedures require revision due to an SSI.[iii] Overall, SSIs occur in between 2% - 13% of orthopedic procedures, varying by procedure type,[iv] and the costs of SSIs comprise a substantial portion of the total cost related to a surgical procedure. One study shows that the payer burden alone of treating SSIs averages $6,745 per original spinal fusion procedure[v], not counting legal and malpractice expenses. Another study estimates the cost of SSIs per original TKA procedure is $3,480.[vi]
“Single-use instrumentation” has been shown to result in a “statistically significant overall decrease in infection rate compared with traditional instrumentation,” including a reduction from 3% to 0.2% in the rate of revision due to infection in total knee arthroplasties.[vii] Another study found that the use of SSP instruments in spinal fusion surgery resulted in a 66% lower infection rate compared to conventional, reusable instruments.[viii]
SSP Instruments Improve Patient Throughput and Reduce Equipment Processing Costs and Environmental Impact
Beyond these critical measures of patient safety and post-operative outcomes, SSP instruments have been shown to shorten procedure set-up time and increase the number of procedures that can be performed per OR, per day.[ix] In TKA procedures, use of SSP instruments reduced OR set up time by 30 minutes and led to “a reduction in turnover time from 15 to 12 minutes, 3 or 4 times per day,” meaning that each day “1 more surgery could be performed.”[x] Another study found that use of SSP instruments allowed one additional case to be completed per OR, per day in 11% of days with an 8-hour operating day and 51% of days with a 12-hour operating day.[xi]
Use of SSP instruments reduced handling, processing, and sterilization-related costs in TKA procedures by an average of $985 per case.[xii] In the case of Open Reduction Internal Fixation procedures, use of a comprehensive SSP instrument set was found to save an average of $1,313 per case.[xiii] Beyond handling and sterilization costs, the reliable availability of SSP instrument kits also “avoid[s] delaying surgery in the case of reusable device unavailability.”[xiv] SSP instruments reduce intraoperative handling time[xv] and overall surgery time.[xvi]
Furthermore, there is a common misperception that single-use instruments increase environmental impact. In fact, “the environmental impact of [SSP instruments] was significantly lower [than reusable instruments] in all studied impact categories” including overall environmental impact, plastic waste, and attributable greenhouse gas emissions.[xvii] The energy use of sterilization and quantity of disposable plastic wrapping (roughly 250g, or 8.8oz per tray) required by reusable instruments were major drivers of this outcome.[xviii] Use of modular SSP instrument kits further reduces environmental impact.[xix] The second-order impact of reduced infections due to the use of SSP instruments—and the subsequent avoidance of additional treatments and procedures—is an additional and significant environmental advantage compared to reusable instruments.
Overall, when appropriately incorporated into a hospital’s surgical processes, current literature supports the proposition that SSP instruments improve patient outcomes, reduce overall cost, and have a lower lifecycle environmental impact compared to reusable instruments.
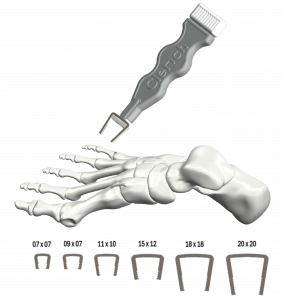
NOTE: Spartan Medical, Inc. sells Single-Use, Sterile, Pre-Packaged (SSP) Micro and Minor Surgical Convenience Kits similar to the products compared in this article. Additionally, a demonstration video of Spartan's Minor Surgical Convenience Kit can be seen below:
[i] In a study involving approximately 210,000 spinal fusion procedures, 1.7% of procedures resulted in a superficial surgical site infection and 4.9% resulted in a deep-incisional surgical site infection (total 6.6%). Risk and economic burden of surgical site infection following spinal fusion in adults. C Edmiston, et al., Infection Control and Hospital Epidemiology, Jan. 2023. Available online at: https://pubmed.ncbi.nlm.nih.gov/35322778/
[ii] Diskectomy SSI rates range from 0.6% to 5%, and instrumented spinal fusion SSI rates range from 6.6% to 8.7%. Postoperative Spinal Wound Infections and Postprocedural Diskitis. S Chaudhary, et al. The Journal of Spinal Cord Medicine, 2007. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2141723/
[iii] Cost analysis an surgical site infection rates in total knee arthroplasty comparing traditional vs. single-use instruments. Siegel, et al. J Arthroplasty2015. Available online at: https://pubmed.ncbi.nlm.nih.gov/26231077/
[iv] Implant contamination as a case of surgical site infection in spine surgery: are single-use implants a reasonable solution? – a systematic review. F Schomig, et al., BMC Musculoskeletal Disorders, Sept. 2020. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7519515/
[v] See Note 1, supra, noting that the increase in commercial payments alone for patients with superficial SSIs was $32,821 (a result in 1.7% of cases) and with deep-incisional SSIs was $93,741 (a result in 6.6% of cases).
[vi] “The cost of a periprosthetic infection procedure is roughly $116,000.” The economic impact of periprosthetic infection following total knee arthroplasty at a specialized tertiary-care center. BH Kapadia, et al. J Arthroplasty 2014. Compare to3% TKA SSI rate at Note 3, supra.
[vii] See Note3, supra.
[viii] Single-use instrumentation in posterior lumbar fusion could decrease incidence of surgical site infection: a prospective bi-centric study. S Litrico, et al. European Journal of Orthopaedic Surgery & Traumatology. Sept. 2015. Available online at: https://link.springer.com/article/10.1007/s00590-015-1692-4
[ix] Single use instruments for total knee arthroplasty. M Romero, et al. Medicinski Glasnik. Feb. 2021. Available online at: https://ljkzedo.ba/mgpdf/mg34/47_Romeo_1321_A.pdf
[x] Id.
[xi] Logistical and Economic Advantages of Sterile-Packed, Single-Use Instruments for Total Knee Arthroplasty. T Goldberg, et al. Health Policy & Economics. Sept. 2019. Available online at: https://www.arthroplastyjournal.org/article/S0883-5403(19)30234-7/fulltext
[xii] Id.
[xiii] Comparative Cost Analysis of Single-use Sterile versus Reprocessed Distal Radius Volar Plate Sets. JA Ly, et al. Arch Bone Joint Surgery. May 2022. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9194709/
[xiv] Single-use versus reusable medical devices in spinal fusion surgery: a hospital micro-costing analysis. C Bouthors, et al. European Journal ofOrthopedic Surgery & Traumatology. Dec. 2019. Available online at: https://pubmed.ncbi.nlm.nih.gov/31350650/
[xv] Processing and Handling Cost of Single-use Versus Traditional Instrumentation for 1 LevelLumbar Fusions. M Galetta, et al. Clinical Spine Surgery, Feb. 2021.Available online at: https://journals.lww.com/jspinaldisorders/abstract/2021/02000/processing_and_handling_cost_of_single_use_versus.14.aspx
[xvi] Life cycle assessment of a disposable and reusable surgery instrument set for spinal fusion surgeries. A Leiden, et al. Resources, Conservation andRecycling, May 2020. Available online at: https://www.sciencedirect.com/science/article/pii/S0921344920300264
[xvii] Id.
[xviii] Id.
[xix] Id.
In the spotlight