Three Key Trends in Healthcare, From Top 100 Healthcare Company CEO
It’s no secret that the healthcare sector is constantly changing, in part because of continual—and almost universally positive—advances in medicine and science.


It’s no secret that the healthcare sector is constantly changing, in part because of continual—and almost universally positive—advances in medicine and science. In the near future, however, the most significant changes in healthcare will (continue to) be driven by economics, not patient outcomes. The following three interrelated changes in particular—all driven by economic factors—will have the greatest impact on the healthcare sector over the next decade. While each has the potential to further marginalize patient care, each also hides a potential silver lining. I’ll do my best to contrast the danger, potential benefit, and interconnection of each.
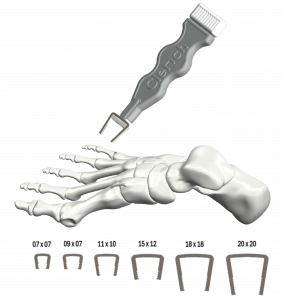
1. Payers transfer long-term outcome risks to providers—in particular for surgical site infections (and how this may drive a single-use, sterile, pre-packaged (“SSP”) implant and instrument revolution)
It’s no surprise, but payers want to pay as little as possible. With more data available now than ever before (at least to some—see below), payers are recognizing the cost of short-sighted care decisions. One particularly timely example of this is the issue of surgical site infections (“SSIs”), which in some areas like instrumented spinal surgery continue to increase in both frequency and cost. Traditional payments to providers cover patient follow-up care over a brief period—often 30 days after a procedure—leaving payers on the hook when an SSIs results in a costly revision surgeries outside of the covered follow-up window . The impact on patient care depends on how providers respond. This payer demand will cut further into provider profits, potentially forcing cost cutting in areas that jeopardize care. But it may also—finally—incentivize providers and manufacturers to more effectively limit long term expenses related to negative outcomes.
One example is the potential to dramatically reduce SSIs, reduce sterilization costs, and improve logistical efficiency through converting to single-use, sterile, pre-packaged (SSP) instruments and implants. Technology and manufacturing improvements have made widespread replacement of reprocessed items feasible, and better data is increasingly proving both the economic and patient-outcome advantages. This is just one example where a payer squeeze can benefit both the bottom line and the patient.
2. Race to the bottom for payments and reimbursements (and how this will help eliminate middlemen that don’t add value)
Likewise, payers and providers are looking to save wherever possible. Increasingly, this means cutting surgical implant prices and reimbursement at all levels. Again, push too far and the results can be disastrous for patients, preventing use of higher quality or innovative technology. While payers’ data-driven, financial focus on the present value of long-term outcomes may protect against cutting too deep, both payers and providers are not wrong: the implant business is highly inefficient. Manufacturers expect markups well over 100%, independent sales reps want ever increasing commissions while hospital systems capitate pricing, and implant distribution models have long been defined by time-intensive rep-surgeon relationships, dominated by megacorps. Markets always have some inefficiency, but the cost of the ‘information processing burden’ to connect product to surgeon in the implant space is beyond extreme. Marketing teams often exacerbate the product: many surgeons won’t leave their rep or won’t leave their “brand” – and as a result the distribution & sales mark-up doesn’t facilitate patients receiving superior products at a lower price. Rather, corporate reps focus on cornering as much of a surgeon’s business as possible, while hospital systems block out competition even when innovative, less-expensive products are often available. The cycle repeats, choice is limited, innovation is stifled, and system incentives remain confusing and misaligned.
Sales reps increasingly add limited value for commodity med-tech, and megacorp / hospital alliances. Eliminating competition will rarely create the most economical technology solutions to consistently achieve the best patient outcomes. Unfortunately, the overreaction of switching to a ‘command-economy’ where large corporate providers or payers force these medical decisions is little better (or nightmarishly worse). The silver lining is that this malalignment presents a massive opportunity for new B2B partnerships between implant manufacturers, distributors, providers, and payers. A firm (or model) that can crack this puzzle could quickly rise to dominance.
3. Data will drive anticompetitive industry consolidation and integration (and unleash an unprecedented labor and antitrust response)
As mentioned above, healthcare data is driving many of these changes—but that data is not freely and openly available to all. To the contrary, one of the chief benefits and drivers of continual consolidation and vertical payer-provider integration is data capture. Increasingly, AI promises to leverage this data to optimize outcomes more efficiently than ever before, but this trend also underscores a fundamental tenet of data science: an algorithm can optimize for profit or it can optimize for patient outcome. It cannot do both. At the risk of being too cynical, here’s a legal reality: corporate healthcare payers and providers have a fiduciary duty to their shareholders to maximize profit. They have no such legal duty to patients—indeed, producing acceptable patient outcomes only serves as a marketing pitch and limits malpractice liability.
Again, however, this potentially grim reality reveals countervailing forces: politicians and regulators will look to address these issues head on; providers—including physicians—will use unionization and other traditional labor tactics; and both public and private antitrust enforcement actions will accelerate. For every action there is an equal and opposite reaction, even if that response is unexpected.
Healthcare is certainly a complicated industry—but more importantly it is a complex industry: each of these factors (and dozens more) form feedback loops with each other. This means that minor shifts in one area can propagate into massive, rapid change industry-wide. While such tectonic changes are never guaranteed, adapting to these changes will require agility and the ability to understand the industry as a ‘system of systems’ now more than ever. At Spartan Medical we believe that our ability to recognize changes in system dynamics more quickly, and take bold action in response more effectively than our competitors is a key and sustainable competitive advantage. I’d challenge you to do the same!
Vince Proffitt is the Founder and President of Spartan Medical, Inc.
In the spotlight